Hyperventilation And Hypoventilation
Overview:
Hyperventilation probably isn’t what you think it is. Hyperventilation is when ventilation exceeds metabolic demands and PaCO2 drops below 5 kPa. The result will be an alkalosis that affects the function of every protein in the body, producing a confusing spectrum of symptoms with a single cause. Shallow, rapid breathing is probably just that, not necessarily hyperventilation.
The importance of CO2
The body’s main mechanism for altering breathing patterns uses CO2 as the trigger, not O2. It sounds counterintuitive, like many topics in physiology, but because CO2 levels determine blood pH and changes in pH fundamentally alter biochemical processes, it’s the thing the body is most interested in regulating. Oxygen comes second.
Whether someone is adequately ventilated can be determined from the partial pressure of CO2 in arterial blood (PaCO2), not from how they appear to be breathing. A patient might appear to be hyperventilating, but in fact be taking lots of shallow breaths and actually hypoventilating. Similarly, when we exercise, breathing increases to get rid of excess CO2; this increase is appropriate (hyperpnoea), since the body is producing increased CO2 that needs to be “blown off”. Ventilation comes down to metabolism: how much CO2 is the body producing, and what alveolar ventilation is required to blow it off to keep PaCO2 at 5 kPa.
Metabolism
If you fuelled the body exclusively with glucose, the amount of O2 consumed and CO2 produced would be the same. This is due to the stoichiometry of burning glucose in O2:

For every molecule of glucose (C6H12O6), six molecules of O2 are required, and six molecules of CO2 are produced. We don’t live on pure glucose though. Imagine if we lived on pure fat instead. The chemistry is rather different (this is palmitin, a common plant and animal fat):

Alveolar ventilation (V̇A)
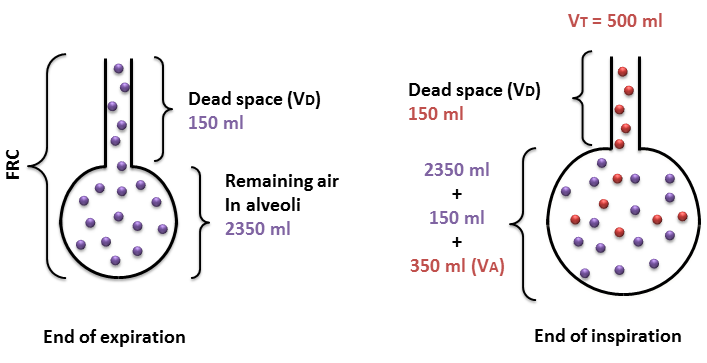
Breathing in and out doesn’t completely replenish the stale air in the lungs. In fact most of the volume of the lungs stays in the lungs, and each breath dilutes fresh air in the functional residual capacity (FRC) of the lung. Furthermore, the air in the conducting airways doesn’t contribute to gas exchange at all and constitutes dead space. At rest, with a typical tidal volume VT; the depth of each breath) of around 500 ml, 150 ml is lost in dead space (VD), and the remaining 350 mL is mixed into the much larger 2350 mL existing FRC. So, it’s not a matter of breathing in, exchanging gases and breathing out. The process of gas exchange goes on continuously, and breathing is just the mechanism for removing a little stale air and adding a little fresh stuff. If we treat the lung as one big alveolus connected to a single airway it works out as shown in Figure 1.
The actual volume of air that reaches the alveoli is tidal volume (VT) minus the dead space (VD):



Gas exchange:
By the time fresh air is diluted down in the somewhat staler alveolar environment (and water vapour is added), PAO2 is 14 kPa, and is mixed with 6 kPa CO2 (equal to PvO2). In fact, you can calculate what the PAO2 should be based on PaCO2 using the alveolar gas equations. If the airways become obstructed, the alveoli become less ventilated and the air in them is staler as a result: PAO2 will drop and PACO2 will rise closer to venous blood levels. Indeed, if the airway leading to a series of alveoli becomes completely obstructed, the partial pressures of O2 and CO2 in those alveoli will equilibrate with venous blood. The process of gas exchange is summarised in Figure 2 below:

Hyperventilation and hypoventilation
Figure 3 below illustrates the relationship between alveolar ventilation (V̇A) and the partial pressure of CO2 (PO2) in the alveoli (PACO2). Remember, under normal circumstances the (PACO2) will be equal to the arterial partial pressure of CO2 (PaCO2)
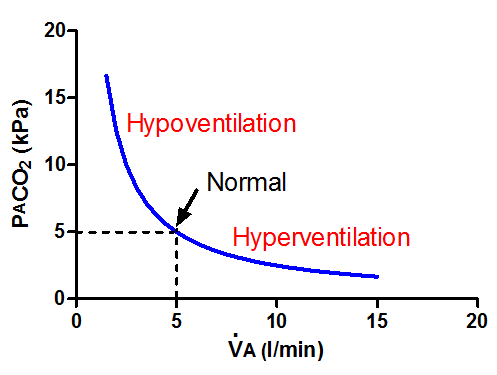
Hyperventilation is excessive V̇A such that too much CO2 is blown out of the body, not breathing too quickly as the word is commonly (mis)used. Hypoventilation is the opposite; you retain too much CO2. So:
