Spirometry
Basic principles
Spirometry is a simple way to test how well air is able to be moved into and out of the lungs. In the most simple test, the patient is asked to take as deep a breath as possible and then exhale as forcefully as possible out of their mouth, for as long as they can. The total volume exhaled is the Forced Vital Capacity (FVC), which is an indication of the functional size of the lungs. This may be reduced where alveoli have been replaced by other tissues such as a tumour or in fibrosis. The relationship between the volume of air expired and time provides an indication of how fast air is able to be exhaled. This will be reduced in a patient with any kind of obstruction in the airways, such as bronchoconstriction.
The diagram below illustrates some volume-time curves, showing how they are altered in both obstructive and restrictive diseases. The volume exhaled in the first second - the Forced Expiratory Volume (1 sec) (FEV1) - is arbitrarily chosen as a measure airflow. The ratio between FEV1 and FVC is used diagnostically to determine whether obstruction or restriction is present.

Compare the normal and obstructed curves above. The FVC for both is similar (this is not always the case - patients vary considerably) indicating that the volume of the lungs is similar. The FEV1 in the obstructed example is much reduced though, indicating that it is more difficult to move air out of the lungs. Such a patient is said to have an airflow limitation, and this is commonly observed in asthma.
Now compare the normal and restricted curves. In this case FVC is considerably reduced, suggesting a lower lung volume. The FEV1 is reduced as well, but only as a consequence of the lung volume being reduced as well. You could think of it as a scale model of the normal curve. Restriction like this may be due to reduced lung volume - as in fibrosis - or due to the reduced ability of the chest wall to expand (due to any number of muscle or skeletal problems).
The FEV1/FVC ratio
The ratio of FEV1/FVC is used to determined whether obstruction or restriction is present. If you consider the restricted curve above, although the FVC is low, the FEV1 makes up at least 80% of this volume, so the ratio would be 80% or greater. This is the cut-off for restricted lung disease. If you compare this to the obstructed case, you can see that the FEV1 accounts for less than half the FVC. This is quite severe obstruction, as anything under 70% is considered obstructed.
It is possible to have both elements of obstruction and restriction in the one patient. In cystic fibrosis, for example, the main problem is obstruction of the airways due to inflammation and mucus. However, after many severe lung infections (which these patients may endure) fibrous scar tissue can build up contributing to lung restriction.
Flow-volume curves
The traditional volume-time curve was used for many years because it was mechnically simple to get a pen to move across paper while a person breathed out into a set of bellows attached to a lever. These days, spirometers have become more advanced and can calculate different parameters. Spirometric data are often plotted as flow-volume curves, which are a little harder to conceptualise initially but are found by physiologists to be more descriptive of lung function. Below are some flow-volume curves to compare with the volume-time curves above.
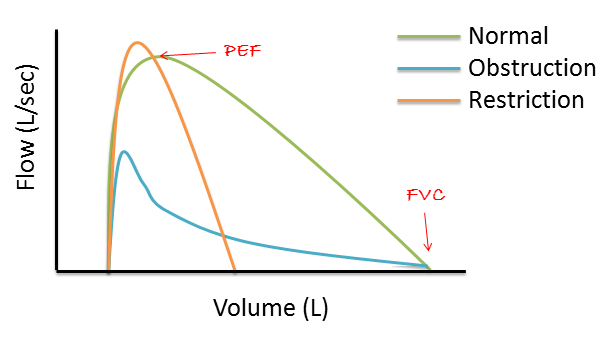
Such a plot is just a different way to plot the same information, after a simple calculation. The volume data are the same as in Figure 1. The flow data are obtained by dividing change in volume by the change in time at that point.
It's probably easiest to concentrate on the volume axis and see how flow changes as the volume of exhaled air increases. In the normal lungs, flow is highest during the initial few volumes of air (as we would expect, given that much of the air should be expired during the first second) and then declines fairly linearly until FVC is reached. By contrast, in the lungs with a restrictive problem, the FVC is reached after much less volume (because these lungs have less volume), but the PEF is similar to the normal lungs. Finally, in lungs with an obstruction, PEF is greatly reduced (as FEV1 is reduced) and flow drops characteristically after the PEF before slowly declining towards FVC.