Neural Control Of Breathing
Overview
The pattern of breathing is probably generated by complex and inter-connected centres in the brainstem which produce bursting of the neurons that fire motor neurons. These motor neurons innervate the diaphragm and other muscles used to generate the pressure differences in the thorax required for breathing. Lesions, as in strokes teach us that our conscious and unconscious controls of breathing are anatomically separate. There’s a lot of neuroscience that we can probably safely ignore.
Central control of breathing
One of the scientists to make a significant contribution to the neuroscience of breathing commented in 1990:
"For
those with a
major interest in other aspects of respiratory physiology and medicine,
the vast amount of information concerning the generation of the
respiratory rhythm presents a bewildering array of facts, in which are
embedded difficult if not obscure concepts whose roots lie in more
remote aspects of neuroscience.”
- Thomas
A Sears (1990) Chest 97, supplement 3, 45S
Not much has changed since then. There are still mixed contradictory and complementary theories as to how the pattern of breathing is generated in the brain and looking into the matter will cause considerable confusion. No two textbooks appear to agree. This is a hideous punishment for students, who are often taught their lecturer's pet theory and examined on it, when it may be of little use later in life.
There’s an oscillator in your head
Neuroscientists are still investigating exactly how the brain generates the rhythm of breathing. There are several models of how different brain regions might interact to produce oscillatory behaviour like this, and the lack of consensus tells us that there’s not much point delving too deep into this field for our purposes. Some physiology texts overlook this aspect of respiratory physiology completely. Pathological and experimental lesions of different brain regions tell us which anatomically-defined parts are important for the functioning of the system, and this is enough to allow us to describe the basic neurobiology of breathing. It’s also enough of a working knowledge to understand how a blow to the head, a stroke or a spinal injury may influence the system, depending on its location.
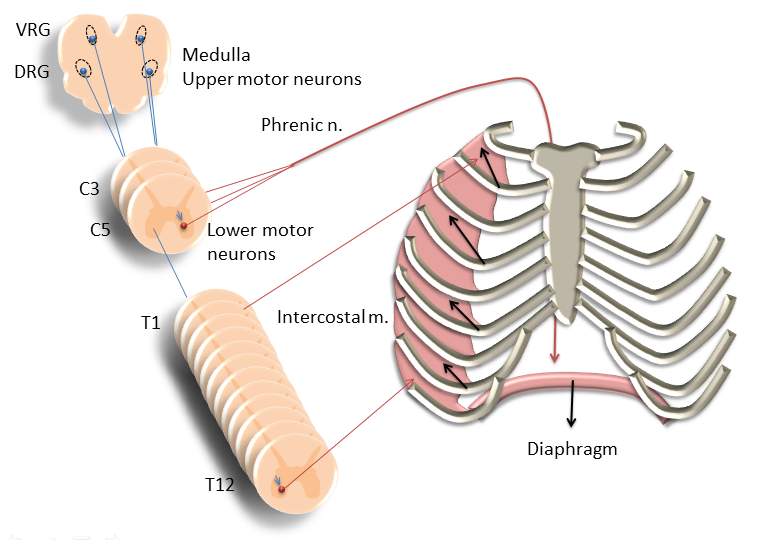
There are two important centres in the brainstem that are important for the genesis of the rhythm of breathing: the ventral and dorsal respiratory groups of neurons. The dorsal respiratory group (DRG) of neurons in the region of the nucleus of the solitary tract appear to initiate inspiration, while the ventral respiratory group (VRG) in the nucleus ambiguus complete inspiration and inhibit the activity of the DRG to initiate expiration. Other centres in the pons also contribute to what we’ll call for simplicity’s sake the respiratory pattern generator (RPG). Parts of this network of interconnected brain regions also receive input from stretch receptors in the lung and information about blood chemistry from chemoreceptors, both in the brain and the periphery.
In normal, resting breathing, expiration requires no muscular effort and lung recoil does all the work of pushing air out of the lungs. Switching off the neural activity in the DRG achieves this. In more forceful breathing, expiration involves the recruitment of the internal intercostal muscles and accessory muscles such as the abdominal muscles.
The muscles of breathing
The muscles used during breathing comprise three basic types:
The diaphragm – the main motor for respirationThe internal (exhalation) and external (inhalation) intercostal muscles
The accessory muscles of breathing
In shallow, quiet breathing the diaphragm does most of the work of breathing. The external intercostal muscles help increase the volume of the thorax pulling the ribs upwards and to side and are brought into action more as the depth of breathing increases. The internal intercostal muscles have the opposite effect and assist in more forceful expiration. Finally, there are several so-called accessory muscles which have other roles (e.g. posture) in the body as their main function but can be used to expand the chest wall. A good example of such a muscle is the sternocleidomastoid which you can feel contract in your neck if you take a sudden, sharp breath. The abdominal muscles are also recruited during forced exhalation.
How it’s wired up
Upper respiratory motor neurons located in the medulla have axons that project down the spinal cord where they synapse onto lower motor neurons. These neurons ultimately innervate the skeletal muscles that drive breathing: the diaphragm, the intercostal muscles and the accessory muscles. The lower motor neurons innervating the diaphragm are located in the spinal cord between C3 and C5, while the motor neurons to the intercostal muscles are located between T1 and T12.
The respiratory system doesn’t just oxygenate the body; it also allows us to speak, whistle, sneeze and cough. The RPG in the medulla and higher, cerebral brain centres interact to control ventilation, achieving different goals. You can hold your breath, if you choose to; you can even whistle whist sitting on your head and your blood gases wont be much altered. However, sometimes the different influences over breathing become disordered. Typically, psychological factors are at play in otherwise healthy people, although hyper- or hypoventilation can result from injury to the brain such as in stroke. Motor neurons from higher – cortical – areas of the brain can completely bypass the RPG communicating directly with the lower motor neurons that innervate the diaphragm and other respiratory muscles. Someone in a highly hysterical state will typically hyperventilate, and be alkalaemic as a result.
What we know from the results of stroke, and in experimental brain lesions on animals, is that the RPG and cerebral control of breathing are separate entities that work together. If a patient has a stroke that impairs the function of the RPG, cortical pathways will regulate their breathing. Such a patient needs to be mechanically ventilated when they are unconscious because they don’t “think” to breathe when asleep. In a rare genetic disorder – Ondine’s curse – the afflicted have a similar defect in the RPG. More commonly, stroke patients lose voluntary control of breathing while the RPG and chemoreceptor control of ventilation remain unimpaired.
The myth of Ondine and her curse is worth looking up, if you need a distraction. Talk about bitter.
Effects of drugs
Drugs that can act in the central nervous system may affect the RPG or its components. Stimulants such as caffeine and amphetamine can produce hyperventilation via their central effects. Some drugs such as aspirin produce hyperventilation through complex metabolic mechanisms. Other drugs may produce hypoventilation by acting as respiratory depressants. Opioids, including those used recreationally such as heroin, will produce such an affect. Respiratory arrest is common in overdoses of such drugs.